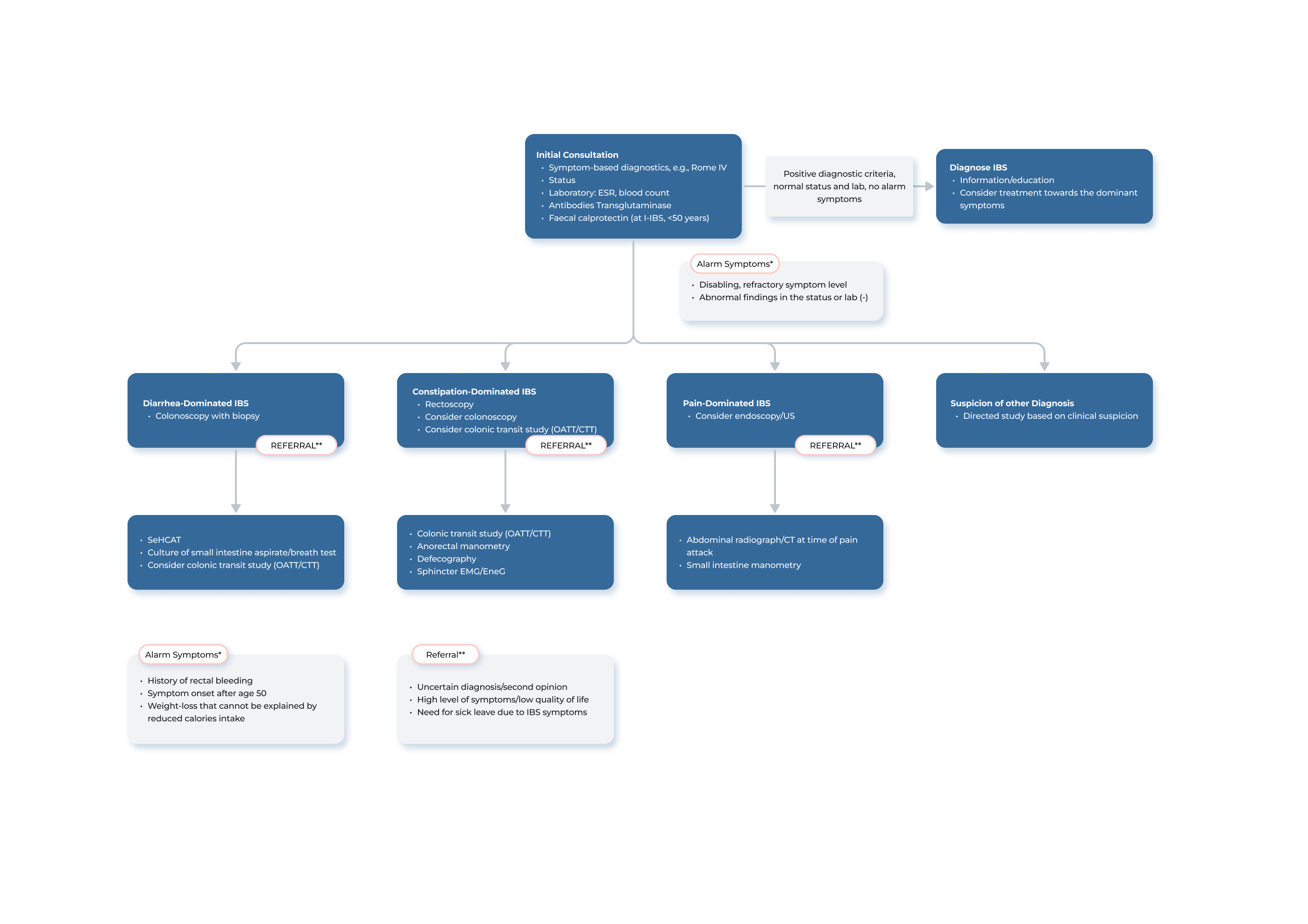
Clinical Guidance for Healthcare Professionals
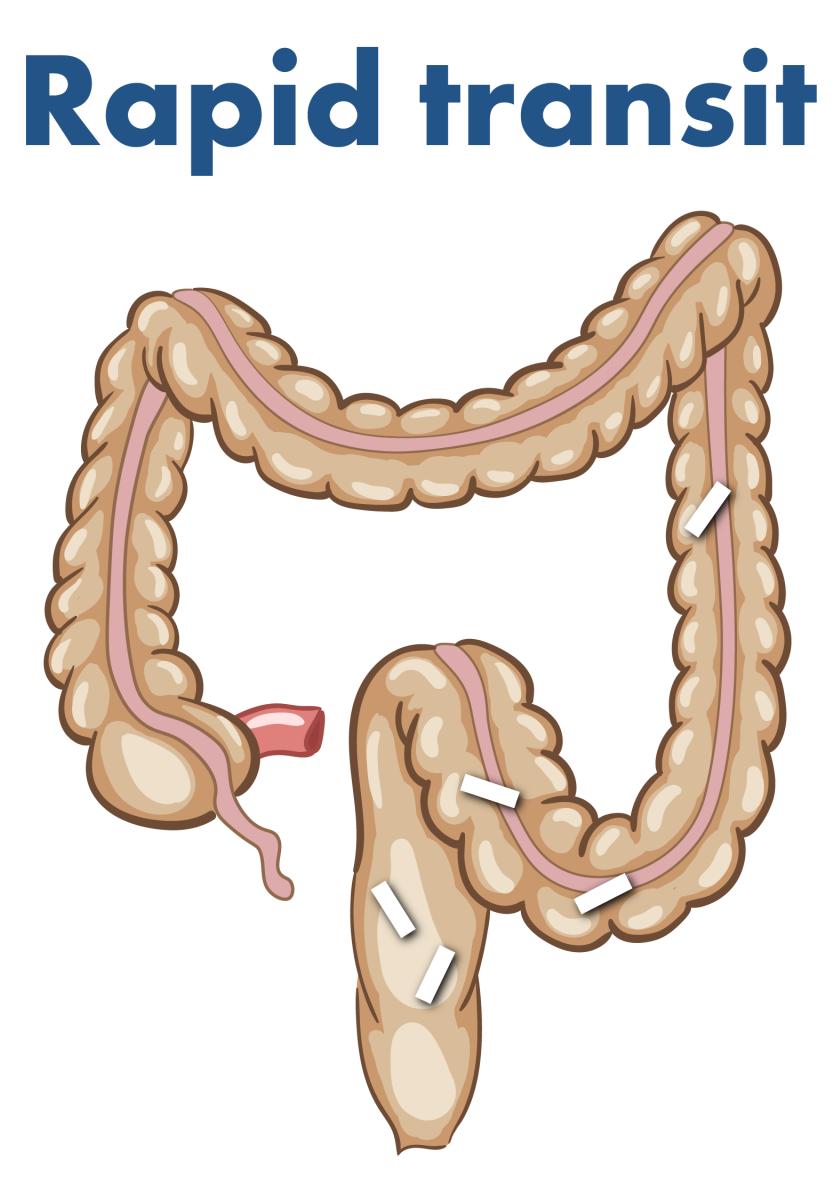
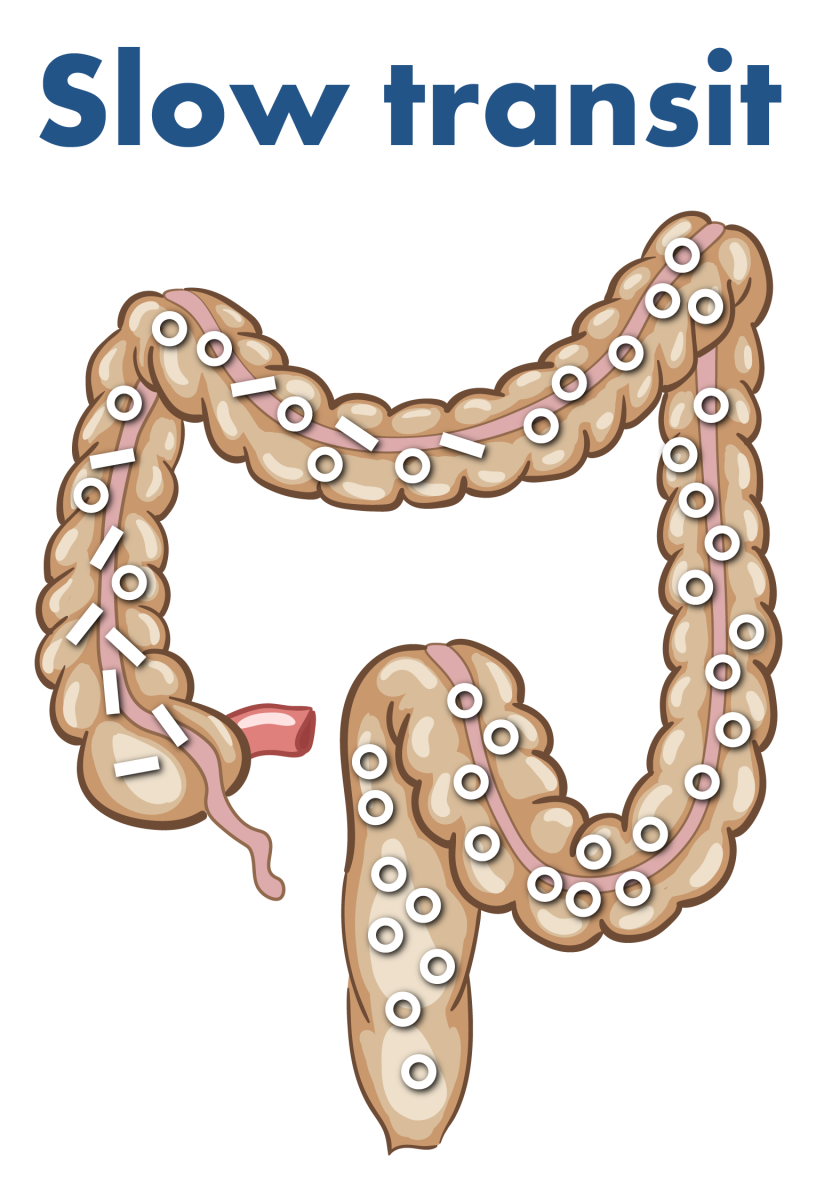
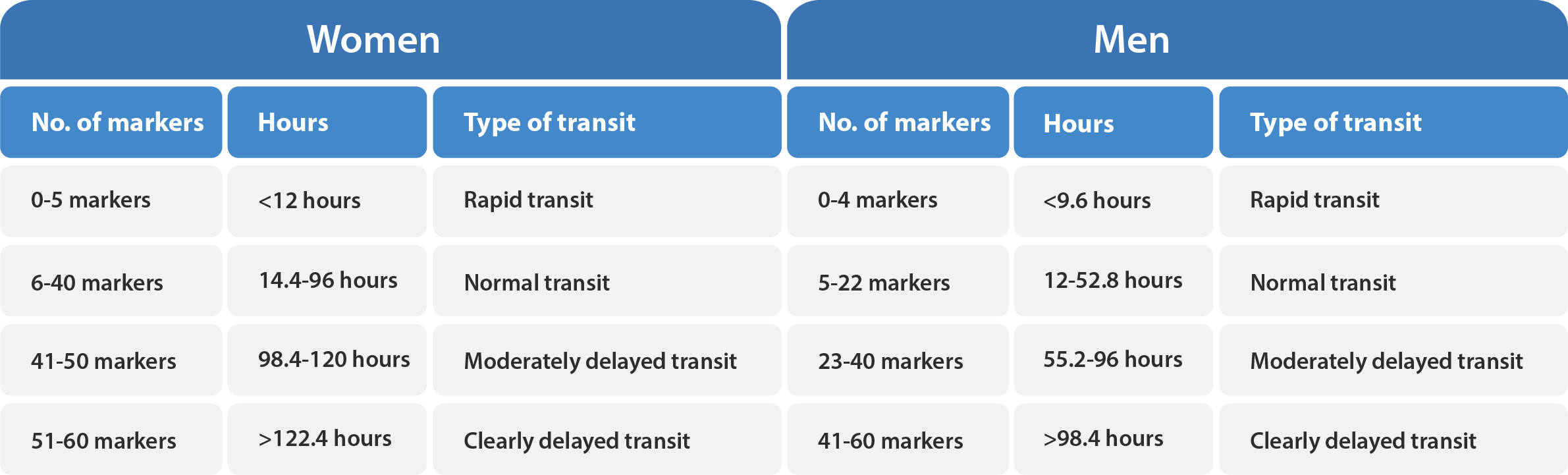
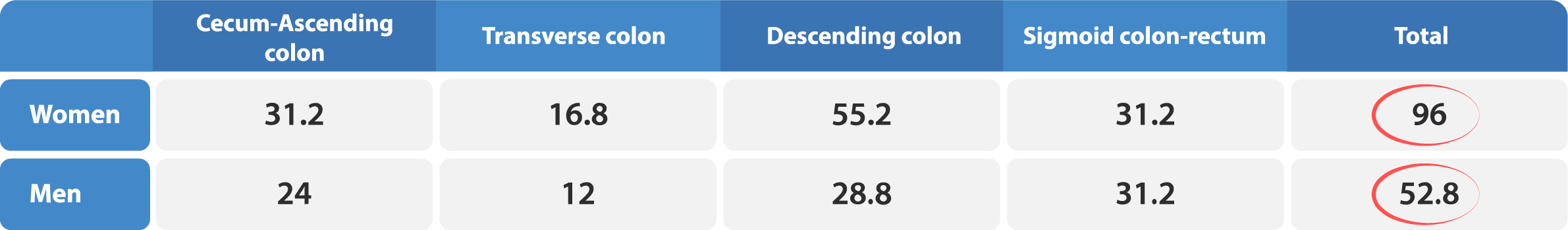
A radiopaque marker study with Transit-Pellets is recommended for clinical evaluation of colonic transit time (CTT) in patients with constipation and irritable bowel syndrome (IBS). The test is indicated to differentiate between normal and slow transit, to assess segmental transit times in patients with delayed total colon transit and to assists in the evaluation of unexplained chronic diarrhea.1
The Transit-Pellets method, also known as the Abrahamsson method, offers a valuable alternative for measuring colonic transit time in patients, as it allows for quantification of CTT while minimizing exposure to radiation. This method is unique in that it is the only single X-ray approach that addresses a range of practical considerations, such as gender-specific differences, both rapid and slow CTT, and the ability to locate dysfunction in various segments of the colon. By achieving an equilibrium between daily marker input and output, this method provides accurate and reliable numerical values for CTT.2
The Transit-Pellets method and Transit-Pellets device can be used to measure:
- Total colonic transit time (in days or hours);
- Segmental transit time;
- Transit time in proximal colon (e.g., in colonic inertia);
- Rapid colonic transit
Illustration of Transit-Pellets marker movement
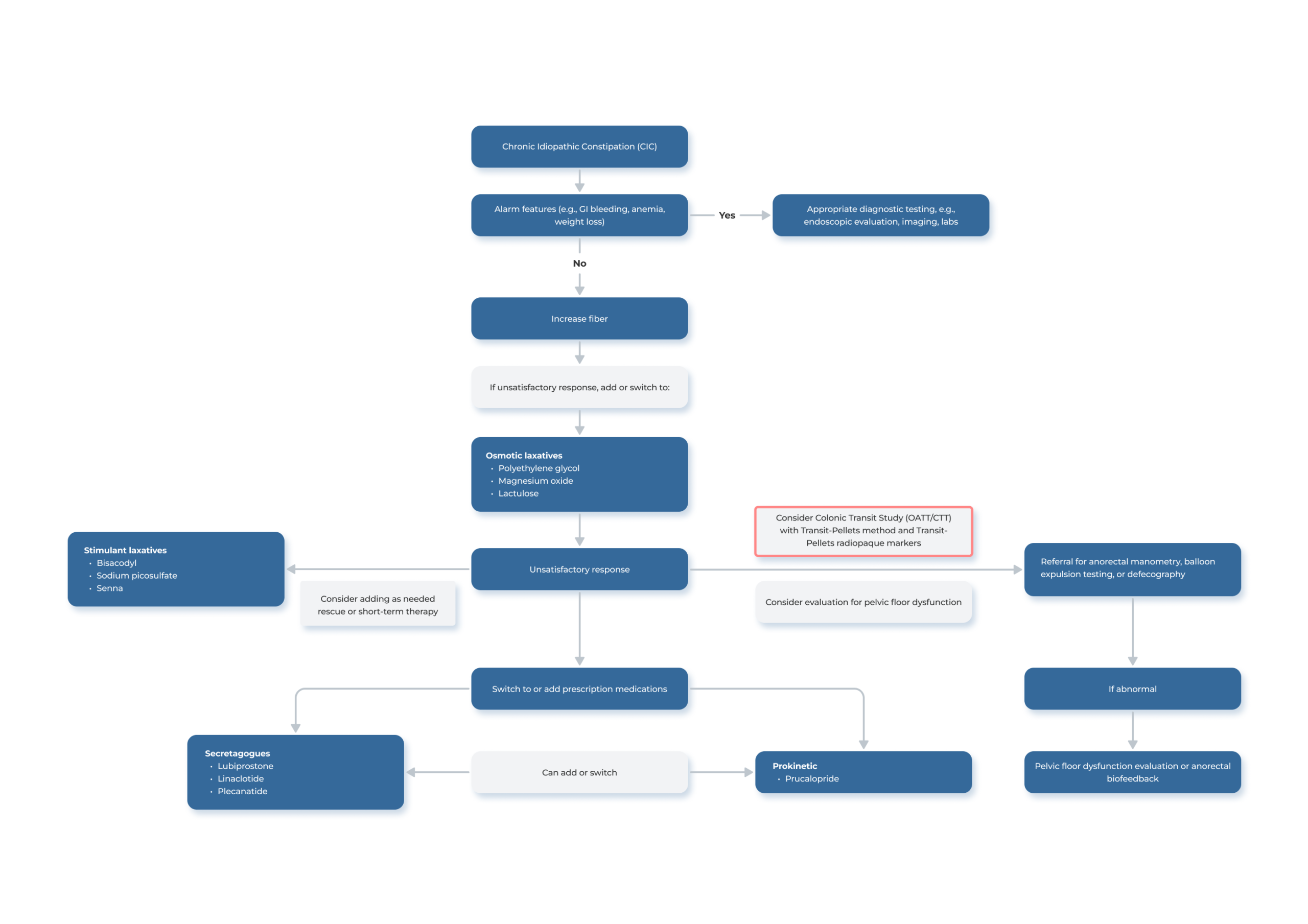
From Diet, Laxatives and Lifestyle Modifications to Colonic Transit Studies
The principles for determining the timing of colonic transit time measurements in relation to treatment steps may vary based on the specific center and the individual physician´s experience. In general, the initial management approach for constipation includes focusing on diet and lifestyle modifications, as well as utilizing standard over-the-counter laxatives such as bulking agents and non-absorbable carbohydrates. If these measures are ineffective, it is common to proceed with a colonic transit study with Transit-Pellets radiopaque markers. Some physicians may also try additional treatment methods, such as the use of saline laxatives or motility-stimulating drugs, before arranging for a colonic transit test with Transit-Pellets.
The referral for the Transit-Pellets procedure may be initiated by a primary care physician or other physician with expertise in treating patients with gastrointestinal conditions. In instances where the case presents complexity or uncertainty, the referral may be directed directly to a gastroenterology specialist for further evaluation and assessment.
Transit studies with the Transit-Pellets primarily address the question, “does the patient have normal or slow transit?”. Further, the assessment of segmental transit time is of paramount importance when evaluating patients with delayed transit. It is advisable that a request is made to the radiology department for the identification of which segment is abnormal.
Clinical Decision Support Tool – Chronic Idiopathic Constipation 3, 4
To download the Clinical Decision Tool for Irritable Bowel Syndrome (IBS), please click HERE.
A Step-by-Step Guide for Physicians and Radiologists
The Transit-Pellets radiopaque markers are prescribed by a physician for use by the patient in the home setting. The provision of clear instruction and information to the patient is a critical component of the procedure.
Transit-Pellets come with an Instruction for Use (IFU) that is available in up to 20 languages. The IFU provides important instructions on the proper use of Transit-Pellets and should be thoroughly reviewed to ensure safe and effective use of the device. You will find it in the footer menu “Downloads” or you can enter it directly via THIS LINK.
In the standard protocol, the X-ray department assumes responsibility for providing instruction and overseeing the use of the Transit-Pellets capsules. It is imperative that patients receive adequate instruction regarding the proper handling of the Transit-Pellets to ensure safe usage. In cases where assessment proves to be challenging, consultation with a gastroenterologist or a specialized gastrosurgeon may be sought for guidance.
For further guidance on the appropriate utilization of the technique and Transit-Pellets capsules, refer to the Transit-Pellets Clinical Instruction for Use. Please be aware that the Clinical Instruction for Use is subject to change. The most current version is always available on this site.
Instructions on Timing and Administration of Transit-Pellets Capsules
The procedure for the colonic transit test using Transit-Pellets includes consuming ten radiopaque markers daily for a period of six days. The recommended time frame between the initial marker consumption and the X-ray examination on day seven is approximately 144 hours.1, 2
Advise the patient to follow the Transit-Pellets capsule regimen as detailed below:
One capsule per day is to be consumed from day one through day five. On day six, the patient should consume one capsule labeled “6:1” in the morning and one capsule labeled “6:2” in the evening. Emphasize the importance of adherence to this schedule to the patient in order to obtain accurate results.1, 2
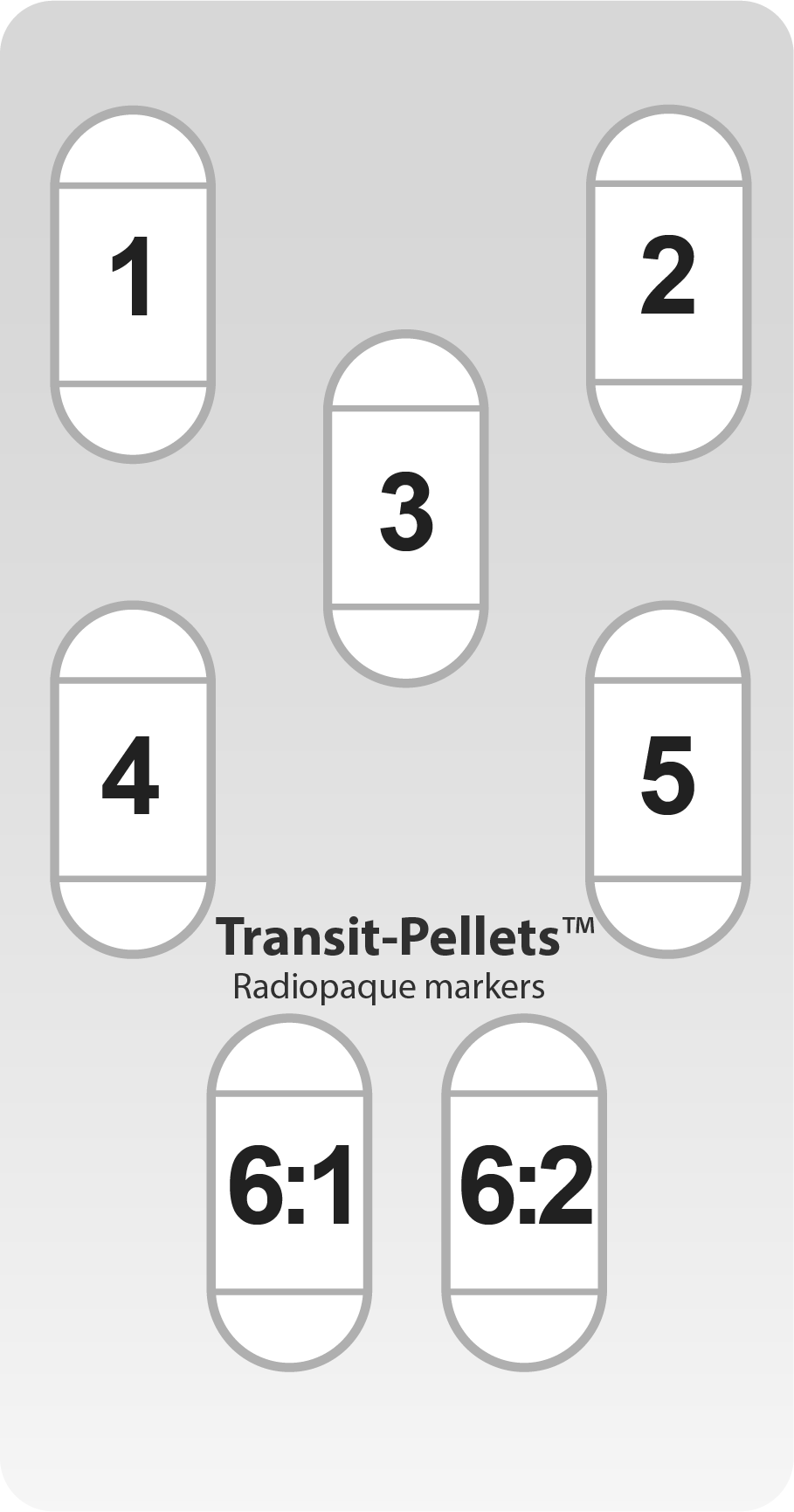 It´s also important that the capsules are taken at around the same time each day.1, 2 For example, if the first capsule on day one is consumed at 8:00 am, the capsules on days two, three, four and five should also be taken around that same time. Additionally, on day six, the capsule labeled “6:1” should be consumed at approximately 8:00 am, while the capsule labeled “6:2” should be consumed around 8:00 pm the same day approximately 12 hours prior to the X-ray on day seven.
It´s also important that the capsules are taken at around the same time each day.1, 2 For example, if the first capsule on day one is consumed at 8:00 am, the capsules on days two, three, four and five should also be taken around that same time. Additionally, on day six, the capsule labeled “6:1” should be consumed at approximately 8:00 am, while the capsule labeled “6:2” should be consumed around 8:00 pm the same day approximately 12 hours prior to the X-ray on day seven.
For patients who may have difficulty swallowing capsules, an alternative method of ingestion can be employed. The contents of the capsules can be emptied into soft foods such as applesauce or yogurt and consumed in that form. It is important to note that the capsules and markers should not be chewed.
Schedule a Plain Abdominal Radiograph or a Fluoroscopy
The X-ray or fluoroscopy on day seven should be scheduled to take place about 12 hours after the patient´s last dose on the sixth day.1, 2 Therefore, the time of the X-ray determines when the patient should take the Transit-Pellets capsules, both in terms of the day they should begin and the specific time they should take them. The following table provides a helpful reference:
| Day 1 (Swallow Capsule 1) | Day 7 (Schedule X-ray) |
|---|---|
| Tuesday | Monday |
| Wednesday | Tuesday |
| Thursday | Wednesday |
| Friday | Thursday |
| Saturday | Friday |
Adherence to the prescribed marker ingestion protocol is crucial for accurate results. However, a deviation of up to an hour in the timing of marker ingestion is permissible, but it is not recommended for clinics to routinely have patients ingest markers in the morning and then perform radiographic examinations later in the day, as this could lead to unreliable results.
Avoiding Laxatives During the Test: Importance for Accurate Results
For the duration of the test, it is important for patients to refrain from using laxatives. Further, while it may not always be feasible to avoid motility altering drugs, it is important to consider their potential impact when interpreting the test results.3
What to Do if a Patient Misses a Transit-Pellets Capsule?
If a patient has missed a Transit-Pellets capsule, it is not recommended to compensate by taking a larger number of markers on a subsequent day. This is because the order of the patient´s transit time cannot be accurately determined, and it is therefore not possible to accurately assess the total and segmental colonic transit time using the markers. If a patient has missed the prescribed intake of markers on two occasions, it may be advisable to try again at a later time to ensure accurate results.
Carefully Selected Raw Materials
In contrast to other radiopaque markers available in the market, which are typically made of plasticized PVC (phthalates DEHP and DOP, and epoxidized soybean oil), Transit-Pellets are composed of 78% Elastosil ® R 401/60 Silicone Rubber and 22% Barium Sulphate.
Why 22% Barium Sulphate?
International experts recommend using a 20-25% proportion of Barium Sulphate in Transit-Pellet markers to accurately measure colonic transit time.4 Using a higher proportion of Barium Sulphate with a specific gravity (SG) above the recommended range of 1.2-1.7 for colonic contents (the dominating food residue cellulose has about 1.5), will lead to inaccurate results and will not yield the actual colonic transit time.
- 0020 Clinical Evaluation Report – Transit-Pellets ver08 (Internal Document). November 2023.
- Abrahamsson, H., Antov, S. & Bosaeus, I. (1988). Gastrointestinal and colonic segmental transit time evaluated by a single abdominal X-ray in healthy subjects and constipated patients. Scand J Gastroenterol. Vol. 23 (suppl 152), 72-80.
- Keller, J., Bassotti, G., Clarke, J., et al. (2018). EXPERT CONSENCUS DOCUMENT. Advances in the diagnosis and classification of gastric and intestinal motility disorders [electronic version]. Nat Rev Gastroenterol Hepatol., Vol. 15(5), 291-308.
- Cummings, J.H., Jenkins, D.J.A., Wiggins, H.S. (1976). Measurement of the mean transit time of dietary residue through the human gut. Gut. Vol. 17, 210-18.